Far from Pain Free
Americans consume over 80% of prescription opioids in the world with only 4.6% of the world’s population. The cost of treating chronic pain ranged from $560 to $635 billion in 2010 and was increasing 9% annually while in 2014 chronic pain shared the top reasons for primary care visits with musculoskeletal pain affecting 1 in 3 or 100 million persons.
Part of the Problem
Neuromusculoskeletal (NMS) pain and dysfunction originating from sclerotomal structures of the spine is a prevalent factor in the growing NMS crisis. Sclerotomes are embryological spinal structures that include bone, facets, cartilage and ligaments. Facet syndrome and facet synovitis are progressive processes involving periarticular and intraarticular inflammation associated with trauma and abnormal joint loading, tracking error, ligament laxity and muscle overstretch. Traumatic causes of facet dysfunction are front and center in current literature, however non-traumatic overstretch due to lack of paraspinal muscle development, poor posture, detrimental ergonomics and lifestyle choices are driving the rapid increase in NMS care. In other words, poor back strength exacerbates a complex evolutionary crisis. Paraspinal muscle mass to spinal length ratios are falling precipitously as we are now the weakest generation in the history of humanity. Spinal weakness, not facet trauma, will drive our profession forward as increasingly unstable facet biomechanics amplify a little known reflex originating from the zygapophyseal joints of the spine.
Facet Pain Management
Is our diagnostic criteria for facet pathology too narrow and do we miss the majority of signs and symptoms, provocative and objective testing and potential benefits in identifying non-traumatic and delayed onset cases of facet instability? Yes. Overstretch or trauma to facet capsular ligament slow stretch mechanoreceptors (SSM) result in ligament laxity6, sclerotogenous pain,(SP) and spondylogenic reflex syndromes (SRS). Innervated through a single spinal nerve or its branches, the SRS was discovered by Kelligren J H (1938-39), formally researched by Wyke and othersand further expanded on by Dvorak/Dvorak in Manual Medicine Diagnostics. The “SRS” term was originally coined by Sutter9 and ongoing research into the underlying pathophysiology of the SRS was published as recently as 20148,.
Spondylogenic Reflex Pain
Acute or chronic facet ligament laxity, mechanoreceptor signaling, reflexive effector target tissue facilitation and progressive pain signaling via neuronal excitability, glutamate signaling8, NGF and peptidergic joint afferents form a complicated relationship between function, dysfunction and pain.
Spinal Stabilization Study
Case Study: 58 year old male with generalized thoracic, lumbar and sacral inflammation, spinal stenosis, intermittent right foot numbness and a history of L4R micro discectomy.
The Operative Word
Can we identify this process in the clinical setting? Yes. To do so, the operative word is “withdrawal reflex”. Facet capsular ligament overstretch will persistently fire SSM and in turn activate the spondylogenic withdrawal reflex. The SRS may or may not be accompanied by sclerotomal pain, but it will always activate or facilitate a multi-synaptic pattern of predefined effector target tissues. These tissues include partial or whole muscles and viscera. Along with myotomal, dermatomal, myofascial, and the pain of local tissue stress or damage; facet sclerotogenous pain is one of a definitive group of pain affects that can be useful for facet differential diagnostics. In the acute stage of facet trauma, local facet pain rarely lasts due to capsular ligament slow stretch mechanoreceptors, or SSM activation occurring seconds to weeks later. When facet capsular ligament SSM activate, they fire at a lower voltage than the facet capsular ligament nociceptors and thus inhibit local pain signaling. Upon clinical presentation, the patient may initially feel varying degrees of focal facet pain followed by seemingly unrelated areas of muscle spasms, joint tracking problems and/or pain days, weeks or months later.
Once Activated
Once activated, the SRS becomes a cascade of reflexive facilitation of extraneous muscles and viscera that create a specific, yet broad subset of pain and dysfunction. This subset is definitive and includes:
(a) Persistent reflexive muscle contractures along the spine with or without facet overload (b) Inflammatory foramina nerve root compression syndromes (facet syndrome), (c) Multiple myotome neurocompression syndromes throughout the spine and body,
C5/C6 SRS and Plantar Fasciitis
(d) Muscle over-facilitation and subsequent reciprocal inhibition, (e) Muscle metabolic fatigue with load capacity deficits, (f) Muscle compartment imbalances with joint tracking error, (g) Attachment tendonitis in over facilitated muscles and (h) Myofascial trigger point development in the below normal core temperature patient (-.8 F° or lower), (i) Viscera over facilitation and (j) Local pain from the reactive histological stress associated with any number of the above stated reactions.
C5/C6 SRS and Plantar Fasciitis
Case Study: 67 year old female patient with plantar fasciitis for 9 months with marginal response to PT. 2 minutes of IR laser therapy was administered to the C5R facet articulation only, resulting in a 2.1 F° drop in target muscle temperature within 10 minutes post treatment. The patient stated a subjective reduction in discomfort of 70%. Equipment: FLIR E8 IR Camera, Lumix 4 laser at 45W SP with 5W CW 650, 810, 910, 1064nm at 40,000 Hz. Frank Jarrell, D.C. 2016
Facet or Disc?
After going down a multibillion dollar path of emphasizing the spinal disc as the prevalent cause of back related NMS problems, the facet joint is coming of age as an increasingly prevalent source of NMS pain and dysfunction. If it sounds complicated, it is and it is not. When viewed as a clearly defined spondylogenic reflex syndrome, it becomes very clear as to how a simple, yet little known reflex can become a powerful source of chaos and pain.
Deriving an SRS Diagnosis
Deriving an SRS diagnosis is dependent upon a comprehensive understanding of facet pathogenesis. An excellent article on Facet Joint Synovitis by E. J. Daily, D.C., D.A.C.B.A.R. can be found in the 3rd. QTR 2016 OSCA (Ohio) On Target publication. It is a great starting point emphasizing medical strategies in managing facet pathology. A less invasive strategy can be derived by rapid and systematic protocols for identifying the SRS in conjunction with infrared imaging and HighFrequency / High Power laser technology. More information can be found at sricert.org.
C1/C6 SRS and Diabetic Neuropathy
Case Study: 68 year old male patient with diabetic neuropathy and left foot muscle spasms. Medications for TII DM were noted. A combined 10 minutes of IR laser therapy was administered to C1L and C6R facet articulation and the dorsal and plantar surfaces of the left foot only. A visible improvement in left foot circulation was noted on IR imaging after 24 minutes with a subjective reduction in foot spasms, painful gate and ataxia. Equipment: FLIR E8 IR Camera, Lumix 4 laser at 45W SP with 5W CW 650, 810, 910, 1064nm at 40,000 Hz. Frank Jarrell, D.C. 2016
Scratching the Surface
There is much to learn about the topic and an article can only be an introduction. Combined with the above information; the included case studies illustrate the practical outcomes of SRS management and how the science and technology can take chiropractic into a new era of predictable, dependable and reproducible and immediate functional objective improvements.
These illustrations include a mix of chiropractic procedures utilizing Spondylogenic Reflex Analysis (SRA) protocols to derive pre and post treatment strategies, FLIR infrared imaging to monitor pre and post outcomes based on thermal dynamics, Chiropractic Manipulative Therapy and/or US Laser Biotech Lumix HF/HP multi-wavelength lasers to generate an immediate therapeutic change in facet status.
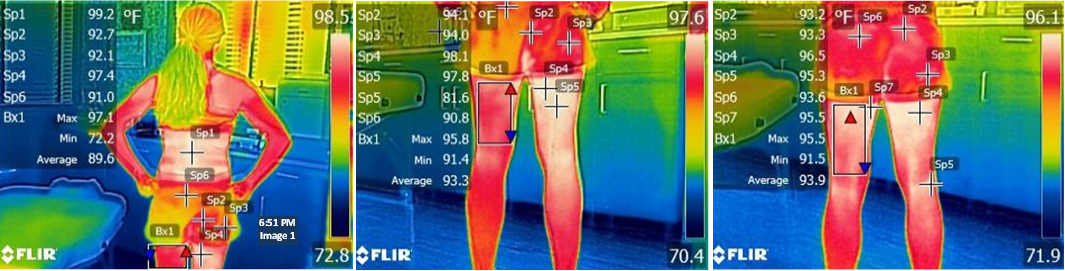
Viewing SRS Derived IR Images
For each case, note the area of complaint, the facet SRS being treated and the length of time on target for laser and/or the limited number of spinal segment(s) adjusted. These samples reflect the impact of facet instability on remote areas. Regardless of where the SRS originates, it becomes a reactive chain of events. Case Study 4 illustrates the remote effects of an SRS in greater detail.
C3/C4 SRS in Elite Athlete
Case Study 4: A seasoned 36-year-old female marathon and trail runner presents two weeks prior to the Imogene Pass Run unable to train. She developed progressive and debilitating right hamstring pain and spasms over the previous year while training for this and other running events. Her complaint progressed into unrelenting right buttock pain, burning in the right posterior thigh and right hamstring muscle spasms. Her MRI/Medical diagnoses included tight hamstring muscle, moderate DJD and L4/5 Grade II spondylogenic spondylolisthesis (SS). She was prescribed 3 months of physical therapy. The Initial steroid injection provided moderate relief while continued spinal manipulation (PTM) aggravated her condition. A second injection proved ineffective. Her initial SRA chiropractic evaluation revealed a spondylogenic reflex syndrome (SRS or primary unstable zygapophyseal joint) at the C4 right and C3 left levels.
Specific chiropractic adjusting to C3 and C4 only along with Spinal Reflex Therapy soft tissue release for the same area resulted in a significant reduction in C3/C4 SRS reflexive psoas muscle contractures aggravating the SS.
Summary
In essence, decompression of the underlying lumbar SS pathology resulted in reduced lumbar facet periarticular hydrostatic neurocompression facilitating L4/L5 myotome to the biceps femoris, gracilis and popliteus muscles. It further reduced metabolic fatigue, spasms, pain and causalgia in the target tissue and increased the patient’s muscle load capacity, endurance and power.
This study illustrates the facet driven SRS neuromechanical compression and soft tissue facilitation cascade. It further illustrates that rapid identification and effective remediation can rapidly effect functional objective improvement. After 1.5 weeks of treatment, the patient not only completed the 17.1 mile run over the 13,114 ft. mountain pass with marginal discomfort; she ranked 1st in her age group and achieved her best time to date.
Images
IMAGE 1 Pre Treatment Low Back Focal Thermal Profile - Sp1 references a focal infrared inflammatory profile at the L4 level with a max temperature of 99.2 F°, well above the average 86-94 F° resting temperature of paraspinal muscle.
IMAGE 2 Pretreatment Posterior Thigh/Knee Inflammation - Sp2 for the right thigh is 98.0 F° compared to left Sp3 at 97.0 F°. Right Sp2 for the right thigh is 98.0 F° compared to left Sp3 at 97.0 F°. Right hamstring metabolism is operating at 1.0 ‘F higher than the left. Sp4 is right illustrates posterior knee attachment tendonitis per popliteus facilitation at 97.2 F°.
IMAGE 3 IR Changes as of 40 Minutes Post Treatment – SP2 reduction of 1.3 F° (95.7 F°), SP3 reduction of 1.6 F° (95.4 F°) and Sp4 reduction of 3.3 F° (93.9 F°) reflect a generalized reduction in inflammation associated with C3 and C4 SRS via a decrease in psoas and paraspinal muscle over facilitation. The GII SS diagnosis was not the determinant factor in performance for this patient. Lumbar manipulation was contraindicated and appeared to destabilize her SS further.
IMAGE 4 SRS Correlate to Hx and Physical Findings - The primary driving spondylogenic reflex (C4R) and reflexively facilitated core muscles are mapped. Note the C4R SRS (red), its psoas muscle facilitation relationship (muscle #11) and its potential for multiple levels of facet neurocompression throughout
the spine.